Dealing with Sundowners Syndrome
What is Sundowners Syndrome?
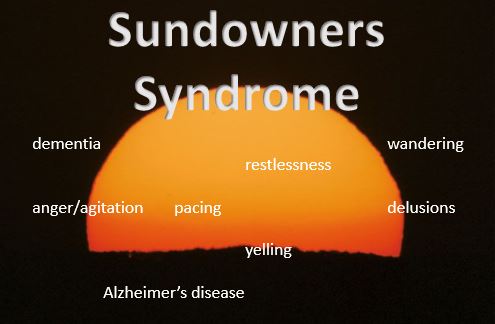
Sundowners describes the phenomena of irritability and other symptoms that occur in the late afternoon and evening in people with Alzheimer’s disease and other forms of dementia. The symptoms a person “sundowning” may experience include restlessness and wandering, agitation, delusions, increased confusion and more.
Many dementia symptoms are simply exacerbated during this period of the day, or your loved one may almost seem like a whole different person when the evening hours hit.
Scientists aren’t sure what causes Sundowners Syndrome. It is likely related to the fading light and perhaps the disturbed sleep cycles and body rythyms caused by dementia. I have always thought that our circadian rythyms and lifelong patterns may play a big role (i.e. this is the time of day when we usually expect transition…leaving work, family arriving home from school/work, preparing for dinner, relaxation, bed). Many times the people sundowning seem to be anticipating that something is supposed to happen, that they should be going somewhere or want to “go home”.
Sundowning can indicate that the person is worn out, in some discomfort, or feeling hungry or thirsty at this point in the day. The person may also be sensing the caregiver’s own frustration or exhaustion at the end of a long day.
How can I manage my loved one’s Sundowners?
- Plan. Anticipate that this can be a tough time of day and schedule accordingly. Don’t plan outings or other activities which might be difficult during this period. Be prepared to provide closer attention and learn ways to redirect your loved one (enlist extra help if needed).
- Prevent. Try to ensure your loved one gets plenty of rest, food and drink. Watch for subtle signs of pain or discomfort. Regularly help him/her to the bathroom. Make sure the temperature is comfortable.
- Soothe. Use soothing music or other activities to create a sense of calm. Find out what works best for your loved one.
- Adjust lighting. Turn on good quality lighting as daylight fades. Consider closing curtains to reduce shadows.
- Provide a safe environment/outlet for pacing and wandering. If your loved one is prone to pacing, you may want to plan walks in a safe area during this time or create a space where he/she can walk around without wandering away.
- Check out our Dementia Symptoms slide show, with practical suggestions for help with wandering and other behavioral symptoms.
- Talk to your doctor about the sundowners symptoms your loved one is experiencing. Sometimes medications can help, or the doctor may need to adjust current medications or address sleep issues.
Contact our eldercare team about dementia caregiver support and resources, dementia home care or respite care and more. For more sundowners, dementia and eldercare resources, sign up to get our free monthly tips.


 Popular Downloads
Popular Downloads


 Get Our Newsletter!
Get Our Newsletter! Mission Statement
Mission Statement

